PR: www.uu.se/en/press/pre...
PR: www.uu.se/en/press/pre...
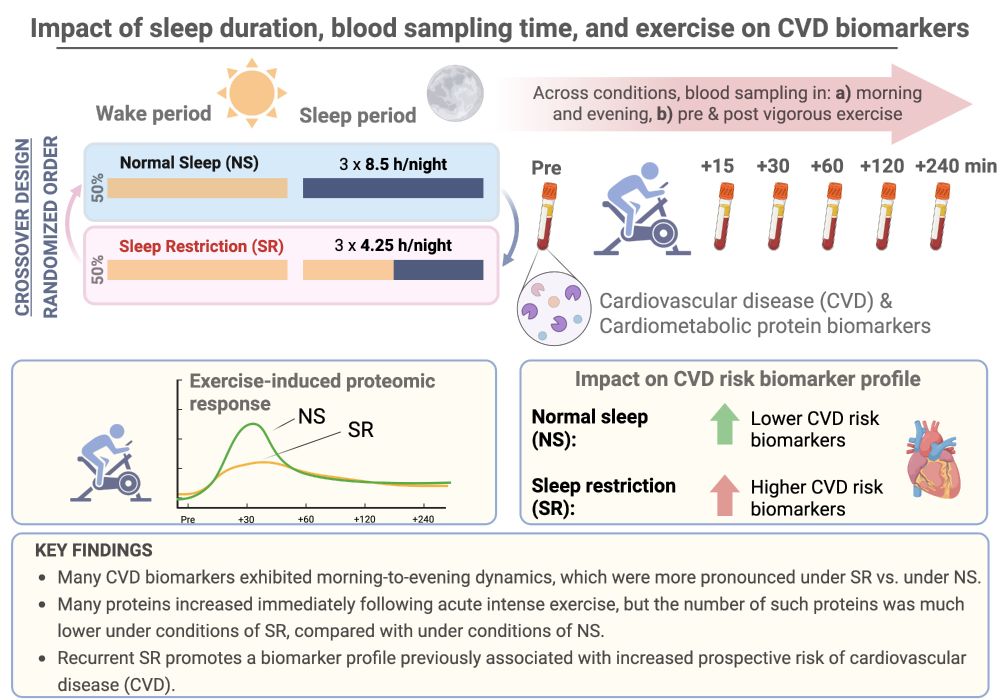
Our findings underscore the need to consider sleep duration, daily sample timing and physical exercise for enhanced precision medicine & #biomarker work
Our findings underscore the need to consider sleep duration, daily sample timing and physical exercise for enhanced precision medicine & #biomarker work

www.sciencedirect.com/science/arti...

www.sciencedirect.com/science/arti...
academic.oup.com/brain/articl...
And earlier in my thread:
Supporting causality, disrupted sleep *4 decades* earlier increases the risk of dementia/AD in humans
academic.oup.com/brain/articl...
And earlier in my thread:
Supporting causality, disrupted sleep *4 decades* earlier increases the risk of dementia/AD in humans
Many reviews cover this – here's our
www.sciencedirect.com/science/arti...
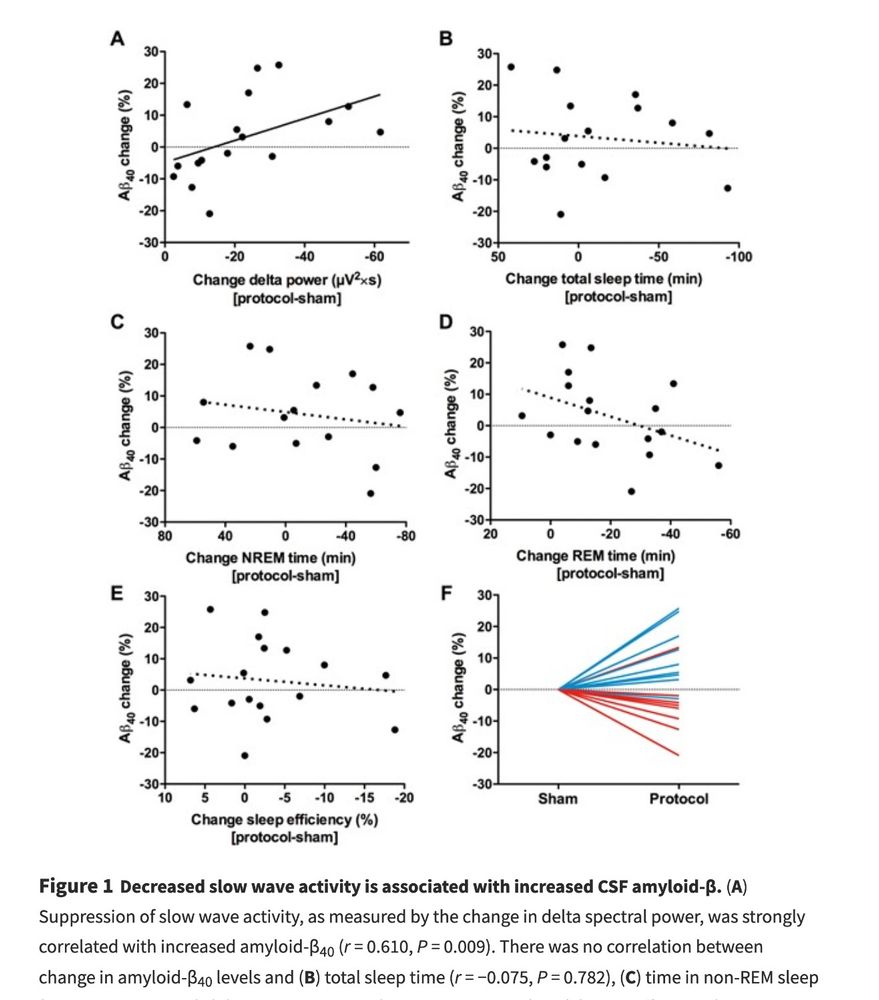
As an example in humans, one night of sleep loss disrupts brain amyloid levels www.pnas.org/doi/abs/10.1...

Many reviews cover this – here's our
www.sciencedirect.com/science/arti...
As an example in humans, one night of sleep loss disrupts brain amyloid levels www.pnas.org/doi/abs/10.1...

In response to our letter: www.thelancet.com/journals/lan...

In response to our letter: www.thelancet.com/journals/lan...
www.sciencedirect.com/science/arti...
This argues against reverse causation as Livingston et al. favor.

www.sciencedirect.com/science/arti...
This argues against reverse causation as Livingston et al. favor.
But as I have highlighted earlier (on X at the time of the publication) most sleep disorders — such as the highly prevalent insomnia — are based on subjectively impaired sleep.
But as I have highlighted earlier (on X at the time of the publication) most sleep disorders — such as the highly prevalent insomnia — are based on subjectively impaired sleep.
- Hai et al. 2022 journals.sagepub.com/doi/full/10....
- (this one from this year), by Jones et al. www.sciencedirect.com/science/arti...

- Hai et al. 2022 journals.sagepub.com/doi/full/10....
- (this one from this year), by Jones et al. www.sciencedirect.com/science/arti...
- Gao et al. 2023 www.sciencedirect.com/science/arti...
- Wang et al., 2022, for night shifts www.frontiersin.org/journals/neu...
- Lee et al. 2023 www.frontiersin.org/journals/pub...

- Gao et al. 2023 www.sciencedirect.com/science/arti...
- Wang et al., 2022, for night shifts www.frontiersin.org/journals/neu...
- Lee et al. 2023 www.frontiersin.org/journals/pub...
- academic.oup.com/sleep/articl... and
- www.sciencedirect.com/science/arti...
- academic.oup.com/sleep/articl... and
- www.sciencedirect.com/science/arti...

