Interested in physiology, medical education, LGBTQ+ health, and the kidneys.
Skeets are my own/not medical advice. 🏳️🌈
#ClinicalTrialsDay #NephSky
👉 www.bbc.com/news/uk-engl...

#ClinicalTrialsDay #NephSky
👉 www.bbc.com/news/uk-engl...
It made the ruling using the Republican-passed "health care freedom amendment" meant to overturn Obamacare!
Subscribe to support my journalism.
You'll want to read this one.

It made the ruling using the Republican-passed "health care freedom amendment" meant to overturn Obamacare!
Subscribe to support my journalism.
You'll want to read this one.



A 🧵
#PhysiologyFriday #MedStudentSky #OncSky
A 🧵
#PhysiologyFriday #MedStudentSky #OncSky

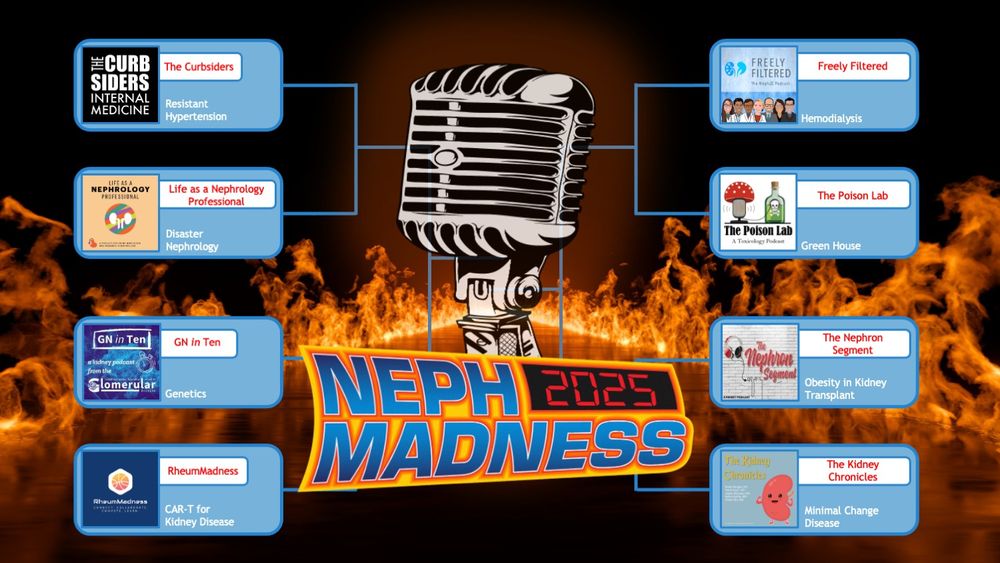
Topics include:
- Resistant Hypertension
- Obesity
- Green House
- Minimal Change Disease
- Disaster Nephrology
- Genetics
- Hemodialysis
- CAR-T for Kidney Disease
Looking forward to the fun and learning with all of you!

Topics include:
- Resistant Hypertension
- Obesity
- Green House
- Minimal Change Disease
- Disaster Nephrology
- Genetics
- Hemodialysis
- CAR-T for Kidney Disease
Looking forward to the fun and learning with all of you!
A🧵
#PhysiologyFriday #MedStudentSky #MedSky #Skytorial #OncSky
A🧵
#PhysiologyFriday #MedStudentSky #MedSky #Skytorial #OncSky
@gudnephron.bsky.social
#NephSky #MedStudentSky
@gudnephron.bsky.social
#NephSky #MedStudentSky
Immediate intervention is crucial.
A 🧵
#PhysiologyFriday #Skytorial #MedStudentSky #OncSky
Immediate intervention is crucial.
A 🧵
#PhysiologyFriday #Skytorial #MedStudentSky #OncSky
A 🧵
#PhysiologyFriday #Skytorial #MedStudentSky #MedSky #OncSky #IDSky
A 🧵
#PhysiologyFriday #Skytorial #MedStudentSky #MedSky #OncSky #IDSky
A must-know🧵 for medicine trainees!
#PhysiologyFriday #MedSky #NephSky #OncSky #Onconeph #MedStudentSky
A must-know🧵 for medicine trainees!
#PhysiologyFriday #MedSky #NephSky #OncSky #Onconeph #MedStudentSky
This is high yield content on the wards and the boards, so let's dive in!
A 🧵
#PhysiologyFriday #MedSky #NephSky #MedStudentSky #Skytorial
This is high yield content on the wards and the boards, so let's dive in!
A 🧵
#PhysiologyFriday #MedSky #NephSky #MedStudentSky #Skytorial
Welcome to another #PhysiologyFriday
A 🧵
#MedSky #CardioSky
Welcome to another #PhysiologyFriday
A 🧵
#MedSky #CardioSky
Far too often I see IV fluids thrown around with minimal consideration; meanwhile, we'll deliberate for hours about a dose of lasix 🤦♀️
Here are the 10 most common fluid prescription mistakes I see 🧵
#emimcc
Far too often I see IV fluids thrown around with minimal consideration; meanwhile, we'll deliberate for hours about a dose of lasix 🤦♀️
Here are the 10 most common fluid prescription mistakes I see 🧵
#emimcc
Let's unpack 5 common diuretic prescribing mistakes, and how to correct these 🧵
#emimcc

Let's unpack 5 common diuretic prescribing mistakes, and how to correct these 🧵
#emimcc
What happened?
A 🧵
#PhysiologyFriday #MedSky #CardioSky #NephSky
What happened?
A 🧵
#PhysiologyFriday #MedSky #CardioSky #NephSky
What are the physiologic mechanisms underlying these associations?
Welcome to another #PhysiologyFriday!
A 🧵
#MedSky #CardioSky

What are the physiologic mechanisms underlying these associations?
Welcome to another #PhysiologyFriday!
A 🧵
#MedSky #CardioSky
journals.lww.com/academicmedi...

journals.lww.com/academicmedi...

